Insurance denials are how they roll. Can we fight back through social media?
September '23: article from The Philadelphia Inquirer: Doctors and patients try to shame insurers online to reverse prior authorization denials. Click here.
Testimony to Congress from a doctor who was working for insurance companies and became a whistleblower, documenting how insurers care nothing about the patient, but take in premiums, and then find any reason to deny care. Click here.
Example of Poor Quality Insurance: Ambetter
I have a whole page on this issue: drwolgin.com/ambetter. Details there of my impressions as a provider about this insurance product.
With money they save by not approving tests and treatments for patients, they have leftover cash to sponsor NASCAR: click here.
Impact of Corporate Business on Healthcare
I want to re-post an important video about the by-product of corporate control of medicine, from this situation in Washington state. The net effect is loss of quality in favor of maximizing corporate profits, with decisions made without regard to local conditions or needs of the patient, nor for maximizing patient safety. While I'm sure this corporate strategy will be good for short term profit growth, probably driven by a far off CEO who will be in another gig in a year or two, patients will suffer, and plaintiff attorneys will have more work to do to right these wrongs.
Letter to GA Insurance Commissioner asking "What DO you do?"
As a doctor trying to advocate for patients, and this opinion is shared by many of my colleagues, I am increasingly seeing the insurance companies as the enemy.
Look at the insurance business model:
--Take in revenue (insurance premiums)
--(at least theoretically) provide a financial backstop for patients so they don't have exorbitant medical costs should they become ill or injured.
However, insurance companies are first and foremost a "for profit" business, and could not stay in business if their expenses exceeded their revenues. Duh. But, not only do they continue to make record profits, but they have become more aggressive about denying patients access to care to a ridiculous degree. And really, any dollar they spend on a band aid is one less that they can retain as profits.
Recent examples: I had a patient with back pain. I ordered physical therapy. Request was denied. Patient got worse. I ordered MRI. Denied...because the patient had not had physical therapy. (Yup.)
Spine fusion request denied because the patient was a smoker. But one detail: as noted in multiple office visits, patient had quit smoking Jan '22 (8 months prior to request).
While other denials have a little more complexity, we medical providers and our staff have had to spend an exorbitant amount of time fighting insurance company delays and obstruction that, I am 100% sure, if the insurance company executives were the patient, they would not tolerate for a second.
I had a recent instance that put me over the top where my assistant was on hold for over an hour with the patient's Blue Cross/Blue Shield to get a needed procedure approved (which btw was eventually judged as medically necessary). I made a complaint to the Georgia Commissioner of Insurance that this type of delay was excessive, inappropriate, and unacceptable. GA Commissioner wrote back saying they couldn't help (pages 3-5 below), so I wrote a letter back to them, which I'm sure they'll ignore (pages 1-2 below) that I'm sharing here.
My letter to GA Commissioner of Insurance 9/8/22
We are engaged in asymmetric warfare, people, since the insurers can make unlimited contributions to influence legislators (try suing an insurance company. Spoiler alert: you can't), as insurers have all the control, all the data, and no liability. What a great business! (for them, but not for patients). I can't ask another orthopedist what they charge for a knee scope. That would be collusion. But they can share all the data about every detail of our practices.
Though there are likely some doctors who, if a patient has an insurance card and a pulse, will order every test and procedure, but the pendulum has swung too far towards profits and away from patients. As noted in the letter I wrote, I am left wondering if there is a branch of government that does help patients?
So, as one of my favorite surgical techs would say:
I'm just sayin'.
A physician applies to law school. Here is her application essay.
This essay below from 4/7/21, from a physician applying to law school, encapsulated a lot of what is wrong with medicine, was posted on KevinMD.com, a social media site for physicians, with the link to that page here.
I have been a physician for 26 years. I have been a fierce patient advocate throughout my entire career. It never occurred to me that physicians do not have the same rights of citizenship that the very patients I fight for do. I always thought I lived in a democracy. Medicine is not what it used to be. Articles relentlessly speak of physician burnout as though we are responsible for what is happening, but that could not be further from the truth. Other articles look for causes like the EHR (electronic health record). The problems are not the hours we put in – that we signed up for – starting with our third year of medical school, every physician got used to sleepless nights. Every physician has been through call and what post-call days feel like. Regardless of specialty, somewhere in training, there was sleep deprivation. That is not the source of burnout.
It is the progressive demoralization of our hard work to attain our degrees and position. We worked 80 to 100 hour weeks in training absorbing as much knowledge as we could because we knew we were responsible for someone’s life, and after training, we would be the final person in charge. That responsibility weighed heavily on us. We wanted to make sure we were optimally prepared.
Meanwhile, businessmen and women invaded medicine. People with no training came along and decided to tell us what we could and could not do. Though we had years of training, these people, essentially practicing medicine without a license, following some arbitrary protocol on a screen in front of them, would deny the medications and procedures and referrals to colleagues, we, with our training, felt necessary.
Legislators have jumped in, practicing medicine without a license, and codified recommendations into law to add insult to injury. Thus creating an atmosphere of fear on top of the demoralization that has already occurred. Boards of Licensure in Medicine (BOLIM), feeling a need to “protect the public,” yield a heavy hand against any such infraction they can find. Mind you, no due process exists with licensing boards, and no one oversees them. What used to be a correction process has become so punitive and arbitrary that entire careers of good, caring physicians have been ruined. This is not burnout. This is moral injury. This is the denigration of an entire profession. No other higher-level degree profession is put through this kind of scrutiny and questioned at every turn. Demoralization compounds when those who have been through BOLIM processes get dragged through the press – and when BOLIMs continue their onslaught and family ask what you did to deserve this – as though you had to do anything. Even physicians whose complaints are later dismissed find themselves branded when they apply for positions as this information is readily available.
When a BOLIM receives a complaint, they ‘investigate’ it. They act as investigative and adjudicatory arms. They are the investigator, jury, judge, and executioner. There is a huge amount of subjectivity to the process and personal animus is clear. Watching careers ruined has given me a new purpose. This is happening all through the country and needs to stop. Physicians are a balance of empathy and scientific inquiry – the persistent attacks are designed to kill – to demoralize, punish and drive physicians to harm. That makes these licensing boards not only operating outside the law but actually culpable. Driving physicians to suicide is murder. Misusing psychiatry, the press to achieve these ends, violating the right to privacy that everyone else in society has, violating the right to due process, all of these together make them arms of destruction, bodies of harm – not bodies of protection, and they should be held accountable for this harm.
To fix this will take a multi-pronged approach. We need to scrap the current State Boards of Licensure in Medicine and start over. Physicians deserve an open, fair process. We deserve to be innocent until proven guilty. Not every complaint deserves an answer. There needs to be screening. Lay people have no business being on these Boards as there often needs to be careful consideration of complex medical issues. Physicians, like every citizen, deserve due process. Too many physicians have been harmed.
My advocacy now needs to be for physicians, and to do that means I need to go to law school. I am ready for this next phase of my life. I grew up with my fists in the air – I have three older brothers (two of whom are attorneys by training), as is my father. My sons are grown and quite supportive of this next chapter; they, in fact, wonder what took me so long to consider law as a career. I bring my experience, dedication, work ethic, and medical expertise with me.
Cathleen London is a family physician.
About the author:
Cathleen London, MD is certified by the American Board of Family Medicine as well as NBPAS and comes to Door to Door Doctors with years of experience in this area of specialty.
For more information about her organization Door To Door Doctors, click here.
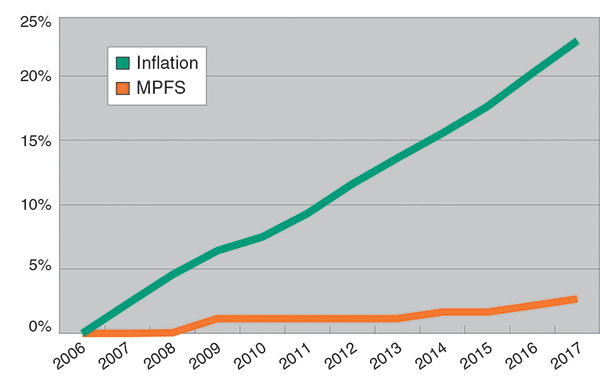
Physician Reimbursements vs. Inflation
(MPFS stands for Medicare Physician Fee Schedule.)
Clearly, physician reimbursements have not kept up with inflation.
Also, other costs of doing business, rent, insurance, salaries, supplies, have gone up.
Here are some thoughts excerpted from an article from 12/14/16 by Dr. Thomas Gaustavino about the current state of our medical system, eloquently stated by him:
The main issue with health care has always been exploding costs.
Here’s where we went off the rails. Sometime around the late 80s the idea became established, especially in political circles, that costs were getting out of hand not due to technology, but because the health care system was providing an inordinate amount of high cost, low-quality unnecessary care just to make money. A vendetta started against the fee for service system to replace it with a more controllable quality based reimbursement system. Whether the politicians did this because they actually believed it or because of political expediency, only they know, although with politicians being politicians I strongly suspect the latter.
…Being in private practice has always been competitive and providing a lot of expensive, unnecessary care is not a good way to keep your customers happy.
(All of the politician proposed) plans failed for the same reason. Obamacare is no exception. Although it did not get a lot of press, and was likely the reason for Obama’s initial claims that families would save money, there were a considerable number of “quality” based health reforms, based on the same false premise that money could be saved if all of that “high cost, low quality, unnecessary care” could be wrung out of the system. Of course, being not true, the exact opposite occurred, and premiums went up. Here are just a few of the other problems that have occurred:
1. The number of health care administrators has exploded compared to the number of providers. This bled money away from actual patient care.
2. Electronic medical records being pushed out prematurely to monitor physicians behavior, causing more problems than it has solved. (see my feelings about this issue here.)
3. Increased government interference in the patient-physician relationship where it does belong, leading to making problems worse. The opioid crisis is a good example.
4. Physicians avoiding complex, difficult, high-risk or uncooperative patients in an attempt to get better quality scores
5. Physicians becoming more super-specialized as they will only do what they are comfortable doing.
6. Increased physician retirement, burnout, and suicide as they try to deal with an ever changing, sometimes conflicting, set of rules and regulations.
To make matters worse, the old problems still exist, such as our runaway legal system, an aging population, and the effects of (patient) irresponsibility. (We need to) consider some realistic and workable reforms, such as dedicating 100 percent of sin taxes to health care or instituting loser pays to our civil tort system.
_____________________________________________________
For an April 2015 article from the Wall Street Journal about the effect of Obamacare causing hospital monopolies, click here. How can there be competition with hospital mergers? Recall the choices here in Albany: Phoebe or Phoebe.
_____________________________________________________
Click here for a link to a March 2015 article by a spine surgeon outlining the routine denials by insurance companies, regardless of facts or medical evidence.
_________________________________________________________________
December ’14: I wrote a letter to Time Magazine in response to an article by Steven Brill:
While I appreciate the great work by Mr. Brill in exposing the inequities and aggressive billing in our healthcare system, for his proposed solution (letting the foxes run the henhouse), he is making some assumptions that would endanger the quality of healthcare, and allow a profit incentive to contaminate the doctor/patient relationship.
Certainly a giant challenge is to align incentives to cut costs and gain efficiency, but some of the issues he cites cannot be generalized. The problem is that there is no litmus test for ethics. Both physicians and hospital administrators could potentially slide down that slippery slope of being influenced by finances and put patient concerns secondary.
Mr. Brill mentions incentives for overtreating and overtesting and used the example of doing chemo on a senior patient. Certainly events occur which could be characterized this way, but the majority of doctors make reasoned decisions and do the right thing. Making the focus on profit of the organization can have a chilling effect.
I work with a health system where more than one physician has resigned instead of following the corporate recommendations on where to refer. While discussing the inefficiencies of the system with another doctor, keeping in mind that getting fired as a doctor can tarnish one’s professional image, this employed physician noted that he has to choose his battles and that “I’d rather have a job than be right.”
Would you like to be a patient in that system?
Mr. Brill also did not mention defensive medicine or the increasing frequency of insurance denials. These days, it is very easy for a bureaucrat in an insurance company (or their employed doctor who has to go by very restrictive guidelines which preclude judgment) who has never seen and will never see the patient, and who can’t be sued for their decision, to routinely deny care. These actions are good for the insurance company bottom line, but bad for the patient seeking treatment.
Sincerely,
Mark Wolgin, MD
Albany, GA
and I got a mention in the letters section!

November ’12:
Here is an article about the financialization of our healthcare system, where insurance companies are becoming “too big to fail,” and healthcare delivery is seen principally as a profit center, instead of having respect for the doctor patient relationship. This article discusses the real danger behind the changes in Obamacare. For link to this article by Nomi Prins, click here.
September ’12:
Here is a link to an article about trends by insurance companies that significantly will decrease the amount of surgical options available to spine patients. Without any disclosure to surgical practices, insurance companies are bundling different aspects of spinal surgeries together to give themselves significant discounts, denying surgeries that previously were covered, putting in monumental roadblocks to care delivery through the pre-authorization process, making appeals more difficult (which will pass on the bill to the patient), and retroactively denying surgeries after they have been authorized and approved.
Article regarding recent trends in care denials by insurance companies, August 2012
This is an article by a spine surgeon, published in Becker’s Spine Review, and I agree with the author’s opinions wholeheartedly, with a direct link to the article here:
Ara Deukmedjian, MD, Founder, Deuk Spine Institute, Melbourne, Fla.: In a spine practice, revenue is directly related to quantity and quality of patient encounters. Surgical and interventional procedures pay more and help offset the losses that office visits (E & M codes) incur for the practice. We have seen yearly reductions in reimbursement for standard spine surgical and interventional procedures by payors. This is primarily due to new spine bundling edits imposed by payors looking to reduce costs. For example during a procedure both codes XXXXX and YYYYY are performed together. If the surgeon or interventionalist received $1,000 for code XXXXX and an additional $1,000 for code YYYYY last year during a specific spine surgery, this year the insurer will bundle codes XXXXX and YYYYY into a NEW code ZZZZZ which pays $1,200. Hence, we receive $800 less every time we perform the procedure this year and going forward. We are no longer able to use XXXXX and YYYYY but are required to use ZZZZZ paying 40 percent less.
These unwarranted bundling edits are usually done for the most common spinal surgeries and since they are so heavily weighted in our collections they have a dramatic impact on overall practice revenue. The bundling is essentially a unilateral “take it or leave it” action by the insurers under the guise of “reducing healthcare expenditures” and supposedly with the cooperation of the AMA and specialty societies; however, these bundling changes occur across all specialties and have been occurring for years without any apparent benefit to the purchasers of health insurance in the form of reduced premiums, deductibles, copays or co-insurance costs. The only stakeholders benefiting are the insurers and their stockholders, certainly not the patients paying the premiums or physicians struggling to survive in private practice with declining payments.
A second major change that has occurred in the last few years is a massive increase in the rate of denials by health insurers for commonly performed spinal procedures that were never denied for the past 20 years and suddenly they are being labeled by insurers (and a handful of “misled” physicians) as “not medically necessary” or “experimental” or “unproven.” Physicians and patients both are very familiar with health insurers ongoing practice of denying coverage for a multitude of prescribed medications and testing labeled by insurers as “not medically necessary”; however, denial for surgery or interventional procedures on the spine is new and indicates a new era of seeming limitless power the insurers have in denying medical care for the sole purpose of reaping in bigger profits.
Of note, insurers are frequently refusing to pay for spine surgery or interventional pain management claiming that the patients only need therapy and psychological counseling to treat their debilitating back and neck pain (that didn’t go away with therapy before); however, there are substantial annual limits on the number of physical therapy visits allowed in a beneficiaries plan imposed by the insurers and it is never enough to cover the cost of all of the necessary treatment when patients suffer from chronic spinal pain. Insurers usually cover only 21 therapy visits a year (therapy is usually 3 times per week) which equates to seven weeks of treatment for a condition that lasts 52 weeks a year. Patients are expected to pay for any required treatment over the allowable per year out of pocket which is difficult to do in a bad economy with high unemployment.
These two major shifts in reimbursement for spine care, reduced payments for services and reduced procedures due to denial of coverage by the insurer, compounded by less disposable income in Americans pockets to pay for escalating individual healthcare costs as a result of the transfer of financial risk from the insurer to the patient, ultimately mean fewer patients will seek the medical care they desperately need and will continue to suffer in pain, miss work, abuse pain killers, have interpersonal relationship difficulties, experience chronic pain related anxiety and depression and a number will only find relief with suicide.
I believe spine practices will see reduced revenue because many patients cannot afford to pay out of pocket for necessary spine care that is not covered by their health insurer and the option of suffering is more affordable to them. High quality specialty care is very expensive to provide and overhead for spine practices is on the rise year after year. The saddest truth here is that we are now able to cure back and neck pain but not without the support of the health insurance industry. Over the last 10 years insurers have successfully mitigated their risk with respect to paying for treatment of chronic back and neck pain by denying or severely restricting coverage of medically necessary (but costly) care of patients suffering with curable conditions, effectively transferring the full cost of treatment to the patient. The vast majority of chronic back and neck pain sufferers are curable with the appropriate care that is diagnosis driven and inevitably requires multi modality treatments including therapy, interventional pain management, chiropractic and occasionally surgery.
The economic downturn will be especially problematic for the millions of Americans suffering with back and neck pain that are under insured (common, insurer refuses to pay the bill to fix their neck or back problem with treatment recommended by their doctor) because their health insurer has been empowered (lobbying, lawmakers) to decide what is” medically necessary” in their care. The idea of a profit driven insurance company in charge of making decisions about what is medically necessary care for you is extremely concerning to me ( less care = more profits). A patient’s personal doctor is that patient’s greatest advocate for health and the decision to proceed with reasonable treatment should always rest with a well informed patient, not an insurance company. Doctors, not insurance companies, take the “Hippocratic Oath” upon graduating medical school. We are bound by its code to always act in the best interest of our patients.
Information for Medicare/Tricare patients
MEDICARE ALERT (November 2011)
Dear Patient,
WE NEED YOUR HELP!
Congress has been postponing making cuts in Medicare/Tricare payments by kicking the can down the road for the better part of the last decade, and now, as of January 2012, the proposed cuts are 27.5%.
The chances are very high that you fit into one of two categories: either you
1) have Medicare (or Tricare for military families), or
2) you know someone who has Medicare, like an older relative.
Recently, a Medicare Payment Advisory Committee (MedPAC) has made another suggestion: to freeze any reimbusement increases to practitioners for the next decade, and for specialists, to lower the reimbursement 6% a year for the first three years. Given that Medicare has been lowering the reumbursements to physicians for the last 15 years, and given that the costs of doing business continue to increase, the net effect of the MedPAC recommendations over the next decade are a greater than 27.5% net decrease in reimbursements to providers.
We really enjoy treating Medicare and Tricare patients and want to keep doing so, but we checked with our landlord, our employees, our suppliers, and our malpractice insurance carrier, and none of them will take a 27.5% discount on what we are paying them. In fact, they all want more money.
Here’s the bottom line: If these changes go through, access to medical care will be severely restricted. Given the rising costs associated with running a medical practice, if these cuts go through, we will have to, as will many other doctors, stop taking new Medicare or Tricare patients.
In order to prevent this threat to access to medical care from becoming a reality, we need your help. We need you to contact your congressmen right away to express your opinions on this matter. Please call Congress today to share your thoughts in this regard. Don’t ignore this issue thinking that somebody else will take care of it. Don’t wait until you or your older family member can’t find medical care. Please call today.
Sincerely,
The Physicians of Orthopaedic Associates.
- Congressional Contact Phone Numbers:
- Congressman Sanford Bishop, Albany Office (229) 439-8067, WashingtonDC Office (202) 225-3631
- Senator Saxby Chambliss, Toll Free 800-234-4208, WashingtonDC Office (202) 224-3521
- Senator Johnny Isakson, Atlanta Office (770) 661-0999, WashingtonDC Office (202) 224-3643
Also, you can contact your Federal Representatives and Senators toll free by using the AMA Grassroots Hotline at 1-800-833-6354 and entering your zip code and you will be connected to the appropriate office.
Also note that the actual percentage of medicare spending that goes to physicians is a small part of the total pie.


Source: American Academy of Orthopaedic Surgeons Research and Health Policy Departments, 2007.
MALPRACTICE REFORM ALERT, April 2010Dear Patient,
Dear Patient,
MALPRACTICE REFORM:
An issue that will affect Georgia patients is Malpractice Reform, also called Tort Reform.In 2005, Georgia enacted malpractice reform which allowed costs of malpractice insurance to be more in line with costs in other states that have enacted similar reforms. As a result, more doctors have chosen to practice in Georgia, which is an issue especially here in the southwest part of the state.For physicians, the risk of a malpractice lawsuit is not evenly spread across all specialties, but is especially high for fields such as orthopedics and spine surgery, and approximately 1/3 of all orthopedic surgeons can expect to be sued in a given year. High litigation rates jeopardize our ability to provide affordable health care, and overuse of expensive tests as part of defensive medicine is a result.
Georgiahas had malpractice reform in place until the week of March 22, 2010, when the Georgia Supreme Court struck down these reforms.
Here is how the court decision may affect you:
-The cost of delivering care to patients, which includes malpractice insurance, will rise, and these costs will have to be passed on to the consumers like you and your family.
-More charges will be generated as defensive medicine will be practiced more intensively.
-For those patients who have fixed reimbursements, like those on medicare and medicaid, the number of openings for patients with those types of insurance will have to be significantly limited.
-Newly trained physicians will be less likely to choose to practice in Georgia and older physicians may choose to retire sooner. Access to care will become a problem.
The physicians of Orthopaedic Associates agree that victims of medical malpractice deserve compensation, but lack of reasonable caps incentivizes lawyers to sue doctors for staggering sums under the guise of malpractice claims, regardless of whether the patients gave informed consent and received responsible, quality care.
We are not sure what the next step will be, but hope that some legislative fix can be applied so that patients don’t lose access to the medical care they so deserve.
We urge you, in the meantime, to contact your state representative to express your feelings on this issue.
In order to prevent these threats to access to medical care from becoming a reality, we need your help. We need you to contact your congressmen and state representatives right away to express your opinions on this matter.
Please call Congress today for Medicare issues and the State Legislature for Malpractice Reform issues to share your thoughts in this regard. Don’t ignore this issue thinking that somebody else will take care of it. Don’t wait until you or your older family member can’t find medical care. Please call today.
Sincerely,
The Physicians of Orthopaedic Associates.
- Congressional Contact Phone Numbers for Medicare Reimbursement Issues:
- Congressman Sanford Bishop, Albany Office (229) 439-8067, WashingtonDC Office (202) 225-3631
- Senator Saxby Chambliss, Toll Free 800-234-4208, WashingtonDC Office (202) 224-3521
- Senator Johnny Isakson, Atlanta Office (770) 661-0999, WashingtonDC Office (202) 224-3643
- State Contact Phone Numbers for Malpractice Reform Issues:
- Governor Sonny Perdue, Office of the Governor, GeorgiaState Capitol, Atlanta, GA30334, Phone: 404-656-1776
- Lieutenant Governor Casey Cagle, 240 State Capitol, Atlanta, GA30334, Phone: 404-656-5030
Representative Winfred J. Dukes, 411-D Coverdell Legislative Office Building, Atlanta, GA 30334, Phone: 404-656-0127 or 920 Highland Avenue, Albany, GA 31701, Phone: 229-432-9891Representative Bob Hanner, 512-A Coverdell Legislative Office Building, Atlanta, GA 30334, Phone: 404-656-7859 or 9610 Plains Highway, Parrott, GA 39877, Phone: 229-623-2841
Representative Ed Rynders, 401 State Capitol, Atlanta, GA 30334, Phone: 404-656-7855 or 423 Martindale Drive, Albany, GA 31721, Phone: 229-888-9928 (Office), 229-436-7455 (Home)
Senator John Dickey Crosby324-A Coverdell Legislative Office Building, Atlanta, GA 30334, Phone: 404-463-5258 or Post Office Box 891, Tifton, GA 31793, Phone: 229-326-6780 (Cell)
Senator Freddie Powell Sims,305 A Coverdell Legislative Office Building, Atlanta, GA 30334, Phone: 404-463-5259 or, 5377 Goose Hollow Road, Dawson, GA 31742, Phone: 229-347-0251
Patient Advocacy Action:
And, for the record, on a recent patient care issue, I was bothered by the way non-emergency transport services would leave a Medicaid patient from a nursing home in our office. Some patient transporters would bring in an older patient in on a stretcher, place them on an exam table (which has no guardrails) and then leave. The situation was not acceptable, since we have no way, aside from the stretcher which they just took away, of even getting that patient to Xray or the cast room.
I wrote a series of letters to the GA Dept. of Community Health, with carbon copies to the Governor, and finally got a response:
